Orthopaedic Services: On the Mend?
The COVID-19 pandemic has led to major disruption of routine hospital services. During the initial outbreak of the pandemic, hospitals reduced elective surgery in the interests of patient safety and to preserve finite resources to meet the immediate healthcare challenge.
Whilst considerable efforts have been made to return elective activity back to pre-pandemic levels, wait times have remained high and as of August 2021 over 5.7 million patients are waiting for treatment.
Delays in elective operations can lead to worsening quality of life. When resuming elective activities, patients are likely to be prioritised by clinical urgency, resulting in lengthening delays for patients with benign, but potentially disabling conditions where there may be less of a perceived time impact. This will result in a deterioration in population health, productivity and have a substantial societal cost.
In October 2021, the UK set out a £6bn plan to accelerate the delivery of operations and other non-urgent care to tackle the increasing backlog of patients requiring care, with additional plans to develop new surgical hubs and technologies to increase elective care capacity by 30% over the next 2-3 years to tackle growing wating lists.
COVID-19 Impact on Orthopaedics | Activity, Patient Volume and Wait Times
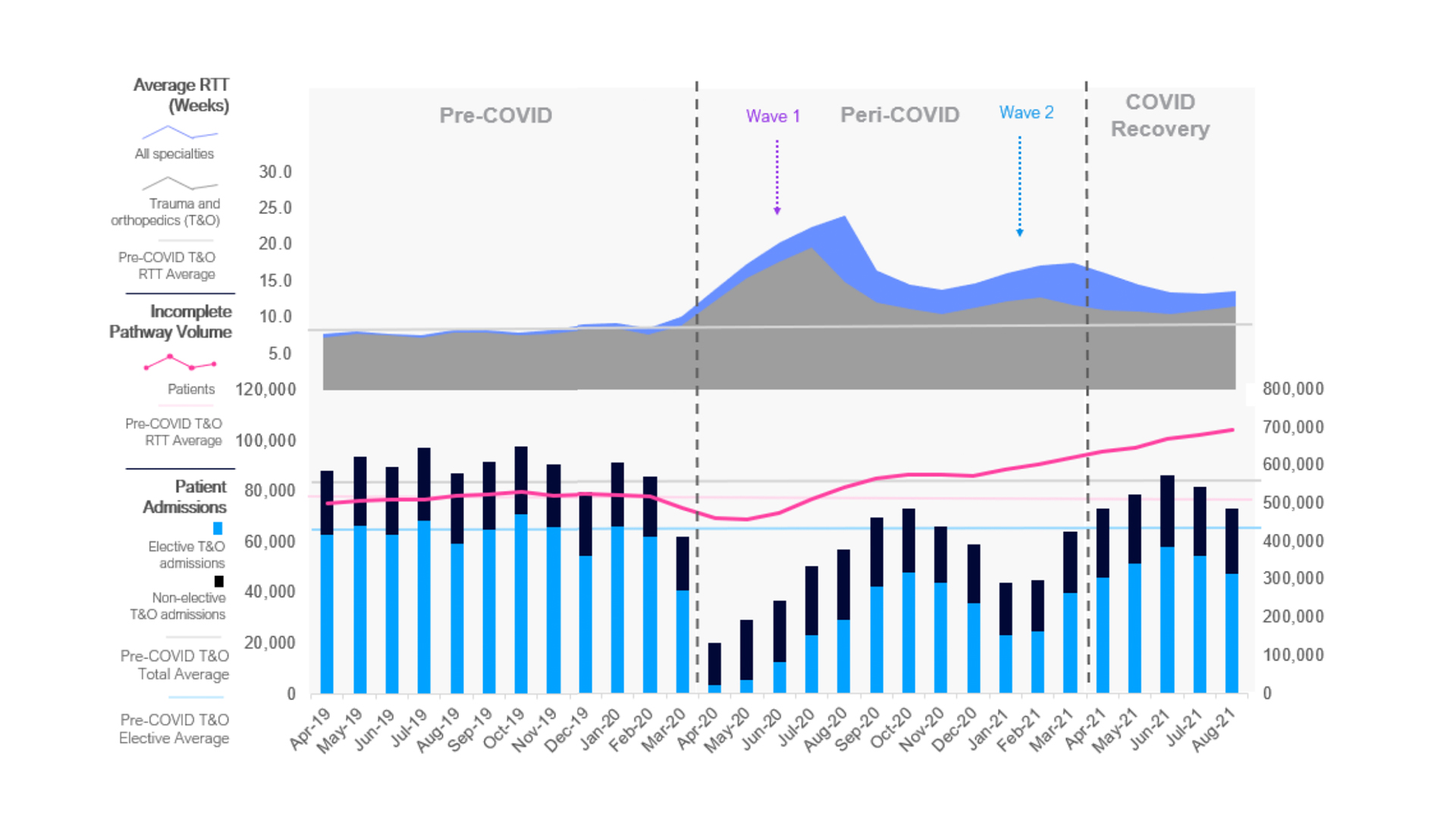
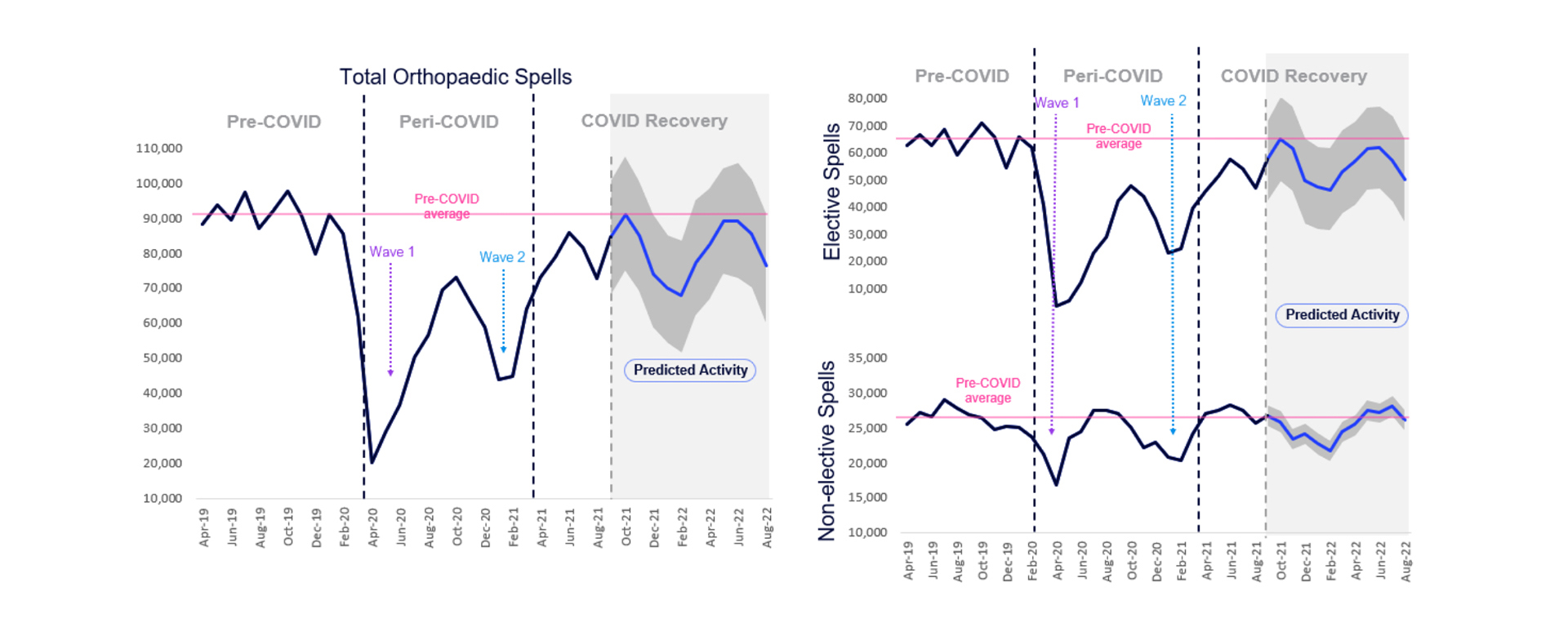
Making up over a quarter of all surgical interventions in the UK, orthopaedics has been particularly impacted by the cessation of elective activity. During the first wave of the pandemic in Spring 2020 elective orthopaedic activity decreased by 93% and remains 17% lower compared to before the pandemic (figure 1).
Orthopaedics persists as the specialty with the highest volume of patients waiting to receive treatment, with a 21% increase in incomplete patient volumes since before the pandemic, from 519,000 in February 2020 to 692,000 in August 2021 (figure 1).
The average referral to treatment (RTT) increased by over 100%, to 18 weeks during the peri-COVID period (April 2020 – March 2021). Whilst the average RTT has reduced since the beginning of the financial year from peri-COVID levels, it still remains 76% higher than before the pandemic (15.5 vs. 8.8 weeks) (figure 1).
Figure 1
COVID-19 Impact on Patients
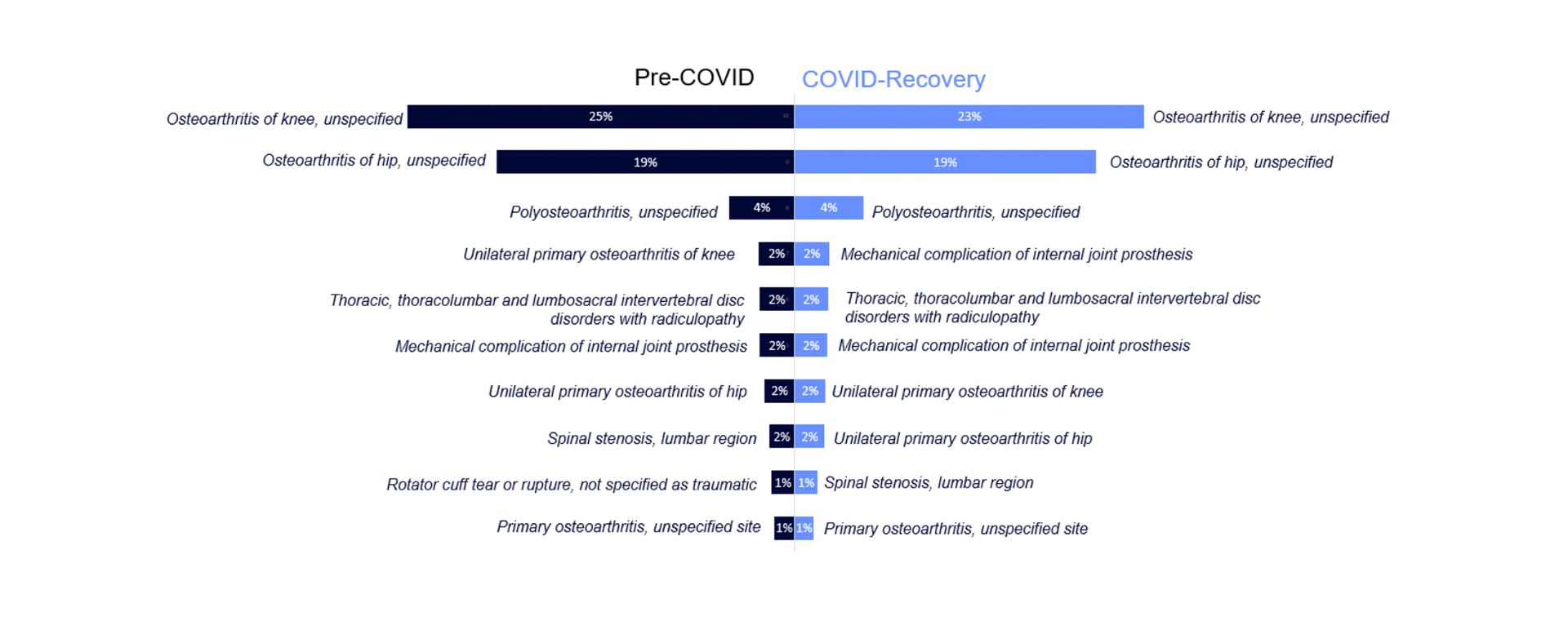
Despite delays in treatment and access to healthcare, at a national level, no significant differences were found in patient characteristics and outcomes between those treated during the pre-pandemic era and those treated during COVID recovery.
Osteoarthritis of the knee and osteoarthritis of the hip continues to be the most common primary diagnosis of elective orthopaedic patients across the study period, comprising 42% of the total patient share over the COVID recovery period (figure 2). Hip surgery had the second longest RTT after foot/ankle procedures, but has the highest procedure volume.
Figure 2
Provider Level Changes in Orthopaedic Activity
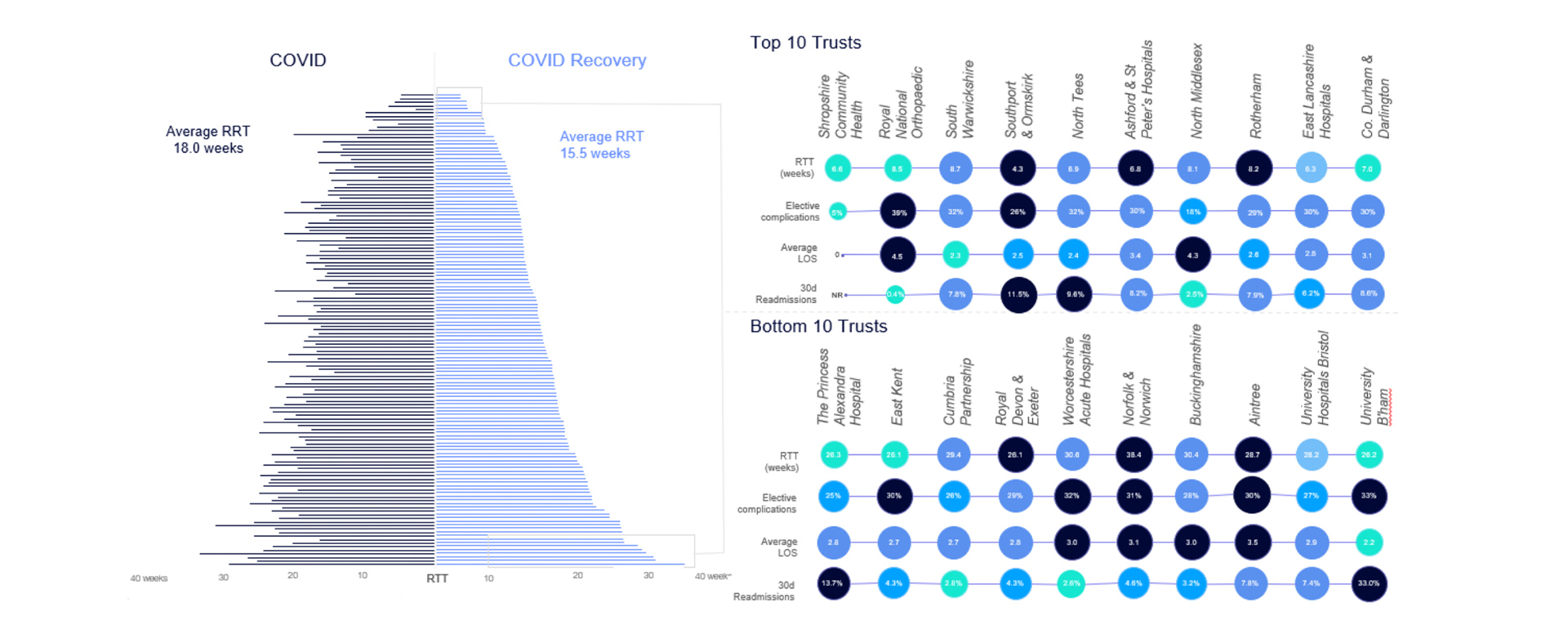
Whilst overall average RTT is decreasing during COVID recovery, there are notable geographic discrepancies in wait times, procedure volumes and patient outcomes (figure 3). In addition, whilst some providers are generating a higher income per bed day, others are experiencing significantly lower revenues per bed day in comparison to before the pandemic.
Figure 3
Predictive Insights for Orthopaedic Activity
Predictive insights generated by the Health Data Science Platform (DSP) indicate that orthopaedic activity may return to pre-pandemic levels over the next year (figure 4).
Figure 4
This predicted activity may not be sufficient to tackle the growing patient backlog resultant from the pandemic. This highlights a significant need for trusts providing elective care for orthopaedic patients to ensure resources are in place to meet this growing demand, particularly in light of increasing patient need. It is essential for services to implement plans to decrease the gap between referral and treatment.
We welcome you to download our complete report here.
