
Predicting Urgent Care Demand
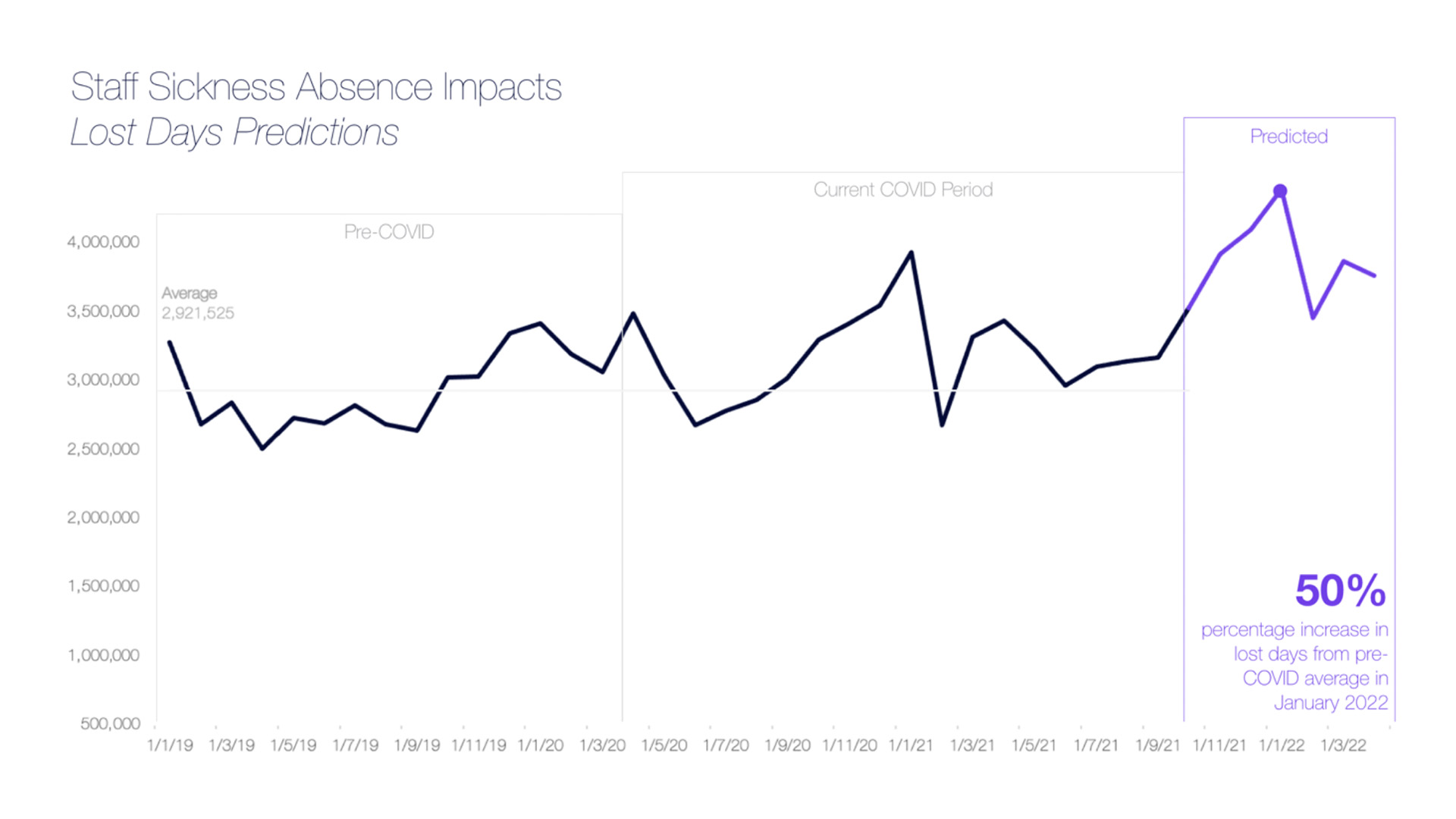
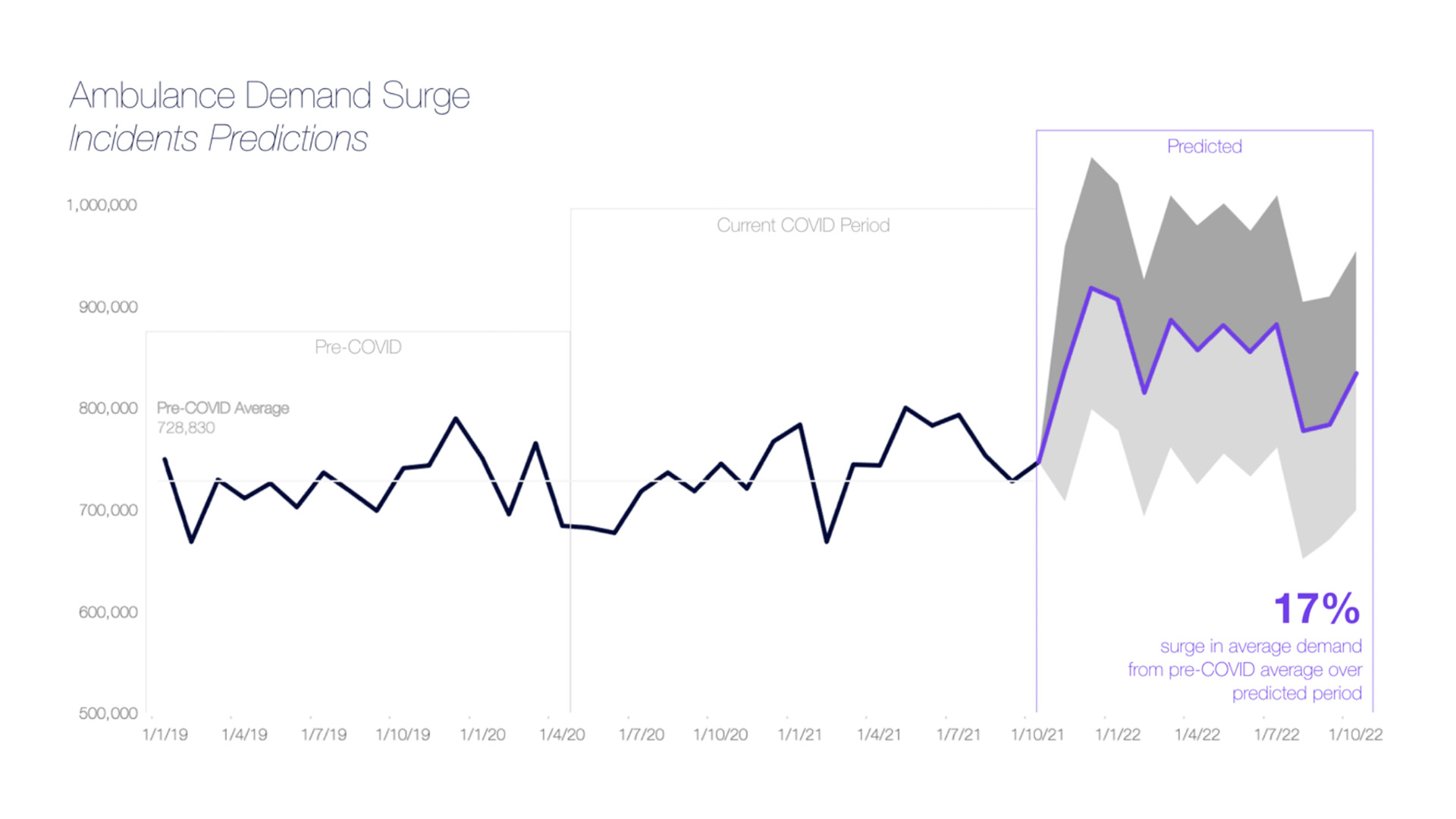
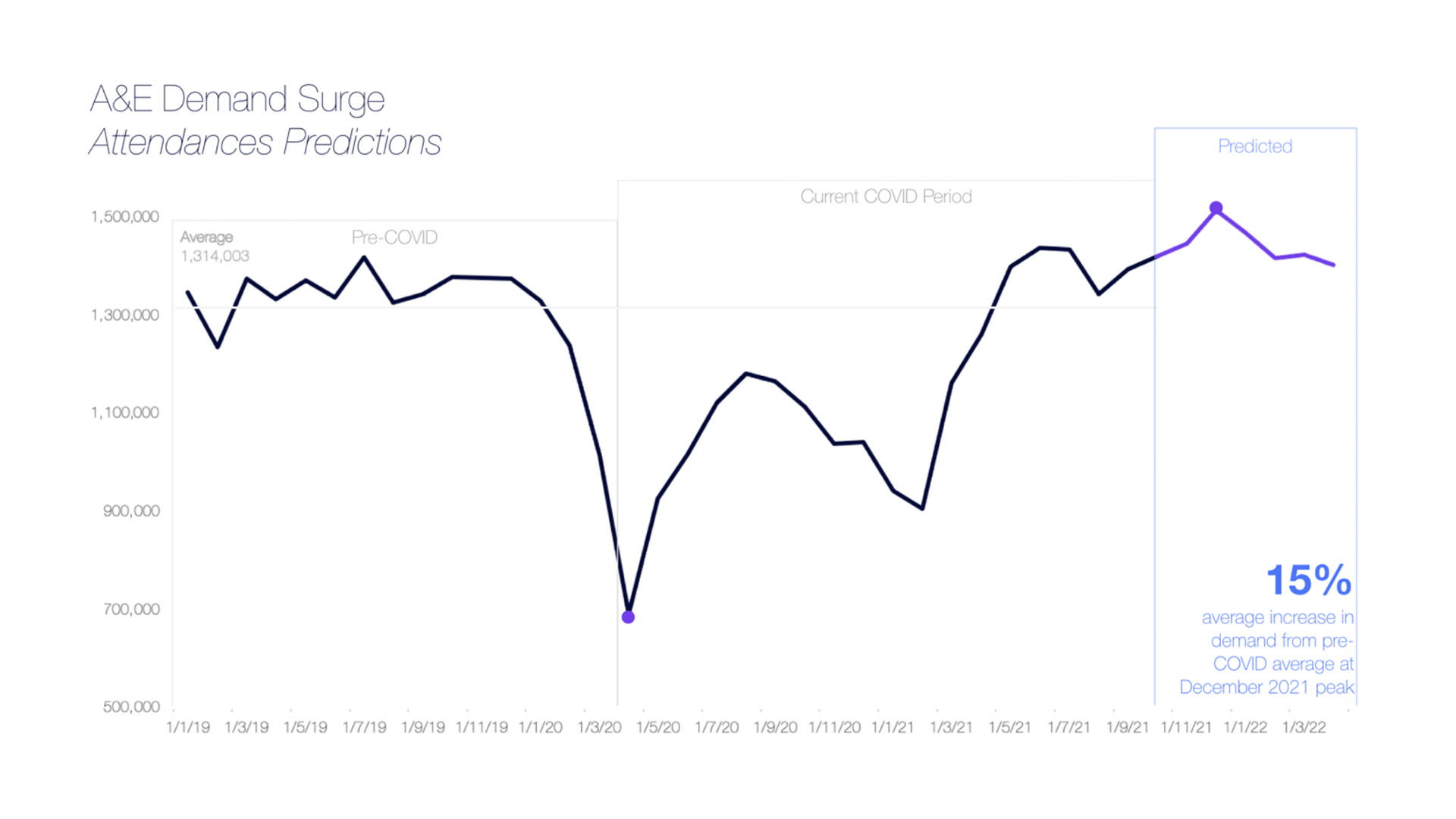
It is starting to get a bit intense and risky for the majority of urgent care providers and systems across the country. As we head towards the holidays, confidential urgent care predictions and capacity modelling show a surge of 47,602 in monthly A&E attendances, and 159,572 in ambulance demand in January 2022. This is compounded with a predicted 23% growth in sickness and absences from most recent rates to January 2022, amounting to over 70,000 staff. Indeed, our AI and data science predictions put the impact of this number at 4.4m days lost by January 2022.
At current admission and occupancy rates, this would mean that most hospitals will struggle to even deliver against a 95% four hour waiting time standard. It goes without saying that this has some serious knock-on effects for the country’s ability to deliver routine care, adjust for urgent care, and reduce the waiting list. It is truly a severe challenge.
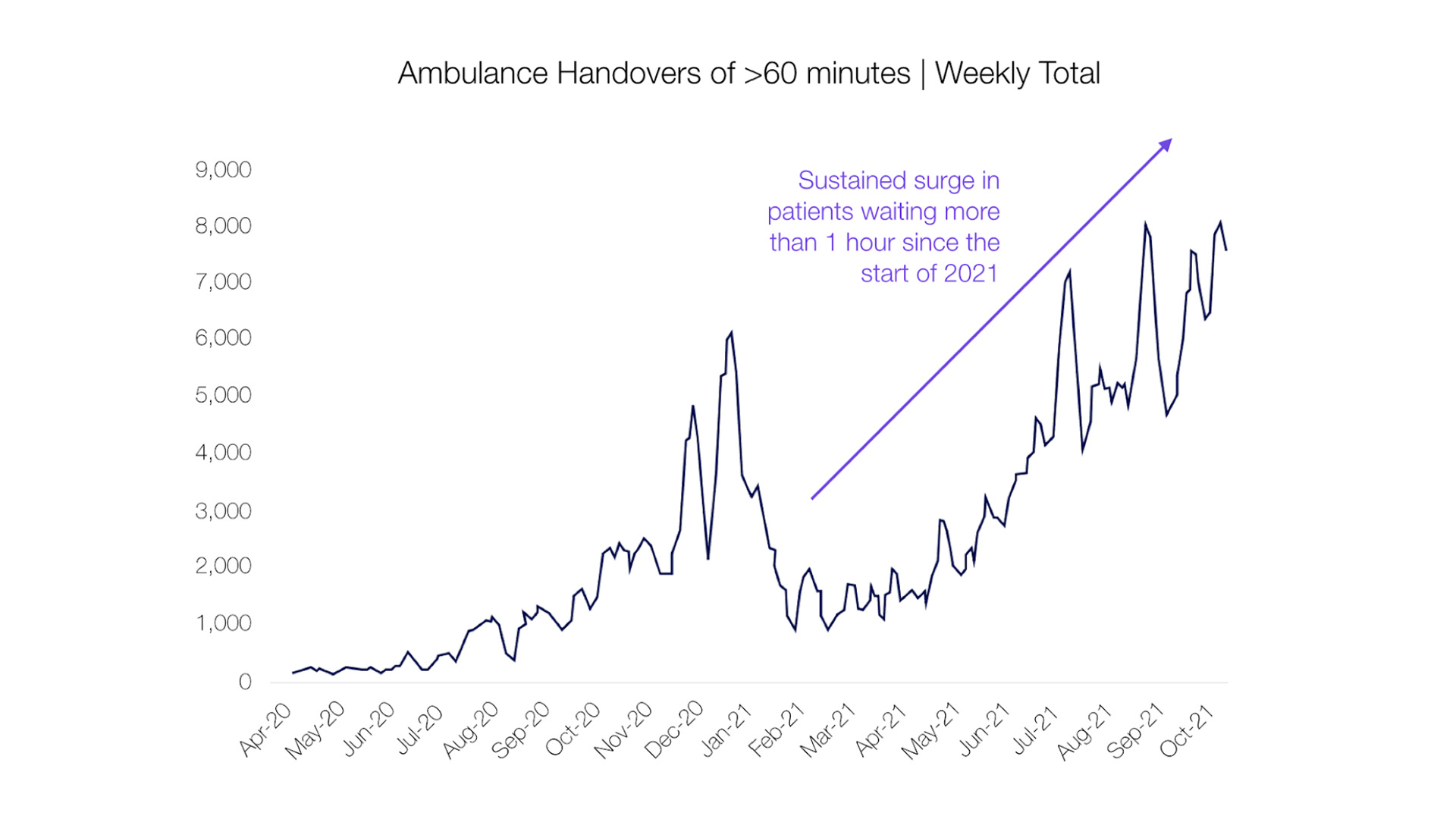
Recent reports have seen more than 7,059 patients waiting over 12 hours for urgent care across England, a 140% surge in trolley waits since September, and an over 260% increase since pre-pracademic levels. Our health system continues to struggle as we head into the winter months, with more than 28,900 ambulance handovers for patients lasting longer than an hour during a four-week period in October. West Midlands Ambulance Service in particular has reported staggering figures, with over 15,000 hours, or 625 days, lost as a result of handover delays to hospitals, due to this surge in urgent care demand.
In light of recent challenges, a statement by an NHS England spokeswoman emphasised: “The NHS has already set out a 10-point action plan to prepare for significant demand this winter and has now gone further by writing to trusts and systems asking for further, system-wide action to be taken to prevent delays with immediate effect.”
Understanding the severe harm patients may face with each delay, the NHS workforce has truly gone above and beyond over the past year, contending with record levels of A&E attendances and ambulance callouts, all while treating more than 470,000 seriously ill COVID-19 patients. As demand shows no sign of slowing, supporting those on the ground and under extreme pressure will be more critical than ever.
So what can hospitals and systems do for some immediate wins?
I, like most of the RwHealth team, originally came from the NHS, and I must say that data, insights, visibility, and predictive analytics were not always in my top three things to prioritise when addressing operational challenges. It often felt like it took too long to get the answers, a feeling I know many of our NHS colleagues struggling through dealing with the surge in complex demand share. However, over the years of delivering complex urgent care and elective programmes for the NHS, I’ve found that not only data, but also deep, predictive, correlated insights and modelling are key to getting quick wins on those ‘what if?’ scenarios.
For example, what if a trust saw 58 more patients in the emergency department or 13 more ambulance handovers in the next 4 hours? What can we do to really deliver as a provider and as a system?
The RwHealth predictive engine and Data Science Platform (DSP) can get you started instantly, as we hold some of your demand, capacity, and complexity data within the platform already. Augmenting this with live local and system data in turn helps to truly support with accelerating appropriate discharges, predictive urgent care demand, and modelling. Check out some of our work at www.realworld.health or email us on info@realworld.health to learn more.

